Dental Cavitation, Root Canal Infection, Dental Implant Infection:
Finding & Treating Hiddemn Dental Infections Can Save Your Life
Hidden dental infections can cause mysterious health symptoms that are not obviously related to the mouth [1]. Unfortunately many of us have these infections in the form of dental cavitations from extracted teeth, root canal infections, and dental implant infections. Our family has seen or consulted with 4 oral surgeons, 8 dentists, 5 osteopaths, 5 chiropractors, 1 oral myofascial therapist, and 1 MD. Lots of Time + Lots of Money = A Few Helpful Pieces of the Puzzle. We are sharing lessons learned from our surgeries, extractions, and experiments, in hopes that others can live a better equation than we have.
Our Stories of Dental Miracles
Symptoms of Dental Cavitation, Root Canal Infection & Dental Implant Infection
Diagnosing Dental Infections
- Tooth Organ Chart
- X-Rays
- Thermal Imaging & AMA
- Self Testing
- Summary – Diagnosing Hidden Dental Infections
Treatment for Dental Infections
- Root Canal Infection & Dental Implant Infection
- Dental Cavitation & Extracted Teeth
- Midline Missing Tooth Options
Case Study of a Friend – Swollen Eyes = Dental Infection?!?
Our Stories of Dental Miracles
“My teeth feel fine, I don’t have any problems, leave me alone!” This is what my husband told me and our dentist for years… Every time we talked about his front tooth #9, which had a root canal. The tooth moved up and down with the seasons of the year. It seemed like there must have been some kind of ‘hidden’ root canal infection, even if he couldn’t feel it. Finally it took two dentists, an MD, and his wife to convince him to pull the tooth. After the extraction, he couldn’t stop raving about how much better his back felt. “I sent you to the dentist, not the chiropractor,” I kept saying. His back immediately felt better, his brain fog cleared up, he had more energy, and most importantly, he did twice as much housework!!
In my case, I had ringing in my ears for as long as I could remember. I battled adrenal exhaustion starting in my 30s despite having great diet, sleep and exercise routines. I had a constant ‘draining’ feeling in somewhere behind my throat, ringing in both ears, was regularly at the chiropractor, and had cold hands and feet. I always thought these symptoms were normal because I had them all of my life. These symptoms miraculously went away after my four wisdom teeth socket (a.k.a dental cavitation) infections were resolved.
I have learned that dental infections can often cause mysterious health symptoms that are not obviously related to the teeth. We have very few practitioners (about two in the USA right now!) who will even consider that the root cause of such symptoms might be in the mouth. Even worse, it is almost impossible for a practitioner to do a root canal, dental implant, or tooth extraction without creating a chronic infection [2,6,7]. Over the course of all of our dental adventures, we have seen or consulted with 4 oral surgeons, 8 dentists, 5 osteopaths, 5 chiropractors, 1 oral myofascial therapist, and 1 MD. Lots of Time + Lots of Money = A Few Helpful Pieces of the Puzzle. The information and videos in this section of Debug Your Health detail everything we have learned (often the hard way!) about dental issues. Hopefully others can live a better equation than we have. I feel so strongly about the importance of ‘hidden’ dental issues that I made a special introductory video:
Symptoms of Dental Cavitation, Root Canal Infection, & Dental Implant Infection
Although not obviously related to the teeth, a baffling list of medical symptoms can be attributed to hidden dental infections [1,6]. These infections can be in a dental cavitation from a previously extracted tooth, a root canal infection, or a dental implant infection. Dr. Simon Yu wrote an article “Wisdom Teeth, Undetected Tooth Infections and Incurable Medical Symptoms [1].” Dr. Kulacz and Dr. Levy wrote a book called “The Toxic Tooth: How a root canal could be making you sick [9].” They list dental infections as an overlooked cause of the following list of incurable symptoms [1]:
- Fatigue
- Headaches
- Arthritic pain
- Heart disease
- Lung disease
- Diabetes
- Osteoporosis
- Insomnia
- Neurological problems
- Hormonal imbalance
- Emotional and psychological disturbances
- Intestinal problems
- Cancer
- Ringing in the ears
- Eye problems
- Other imbalances on the tooth organ chart
Sometimes, applying pressure on the jaw bone above a specific tooth, or in the area around a tooth may cause pain. Often not – usually there is no pain or obvious indication that anything might be wrong in the mouth. No obvious symptoms in the mouth, however, doesn’t mean that there isn’t a hidden infection.
Diagnosing Dental Infections
The most likely places for hidden dental infections are in root canals, implants, and previously extracted tooth sockets. Root canals are performed because the tooth became infected. Unfortunately, bacteria can hide quite easily in a tooth. Every tooth has the three miles of dentinal tubules and accessory canals (ie Tiny Pathways – See pictures in reference [6]). Once a tooth is infected, it is almost impossible to sterilize [6]. There are simply too many great hiding spots for bacteria.
When a tooth is extracted, the body should fill in the space that the tooth occupied with new bone. However, when the periodontal membrane is left behind, this healing doesn’t happen. The bone will heal around this membrane, leaving a hole in the middle. This hole can be empty or filled with dead bone and marrow [7]. The hole is the perfect hiding spot for bacteria, viruses and yeast. The hole is surrounded by bone, so there is no blood flow. The bacteria are protected from the immune system.
Tooth Organ Chart
Hidden dental infection symptoms often follow the Tooth Organ Chart, an example of which can be found in this Tooth Organ Chart. Sometimes this is also called a Tooth Meridian Chart. There are various versions of this chart that have slight differences, but the basic idea is the same. Focal infections in one part of the body (ie a tooth or tooth socket) can travel to and create an infection another part of the body [1]. This may all sound hokey, but I totally underestimated the importance of this chart. It has proven correct time after time.
Dr. Louisa Williams wrote a rather abstract article about dental cavitation surgery. She talks about ‘dental focus,’ and she is right, dental cavitation infections can affect other parts of the body. However, she totally misses the Tooth Organ Meridian Chart. The Tooth Organ Chart is a very simple and clear way to get an idea of which symptoms might be related to hidden infections in the mouth. This chart applies equally well whether it is a dental cavitation infection, root canal infection, or dental implant infection.
In my case I had hidden dental cavitation infections in my wisdom teeth sockets. It turns out that the teeth were not properly extracted 25 years ago. The Tooth Organ Chart lists for the wisdom teeth (#1, 32, 16, 17): heart, small intestine, circulation/sex, triple warmer, shoulder, hand, sacroiliac, foot, toes, middle ear, CNS, jejunum, Ileum, duodenum, anti-pituitary. I had ringing in my ears, cold hands and feet, a hiatal hernia at one point in time, parasites in my intestines (in hindsight), adrenal fatigue (triple warmer), and my sacroiliac joint was almost always unstable and I was often at the chiropractor.
For my husband’s hidden root canal infection, tooth #9 on the Tooth Organ Chart indicates: Post, knee, sacroiliac joint, ankle, sinus, tonsil, pineal, left kidney, bladder, prostate, testicle, rectum. When #9 was extracted, he couldn’t stop talking about how great his back felt. He had twisted and tweaked his ankle several times, and that has not happened since the tooth was extracted. He later had an infection in his genital area (phimosis) and sure enough when we re-checked the socket of #9 after extraction, it was infected – still!
Our experience is that symptoms may not show up on the same side as the tooth. So an infection on the right side might not necessarily show up with symptoms on that side. Often a spinal segment effected by a tooth will cause other spinal segments to try to compensate. The source of chiropractic discomfort may be caused by one of these compensating spinal segments, rather than the original segment listed on the Tooth Organ Chart. I have learned use the Tooth Organ Chart for debugging – if there is a problem with a specific organ or part of the body, I go back and reference the chart. I then test if there might be a problem in the teeth related to that meridian. I also use the chart in the ‘other direction.’ For example, if I get a cavity on a specific tooth, I might test for parasites or a nutritional deficiency in one of the related organs.
Generally we observed that our most obvious symptom of dental infection was musculoskeletal. If we were going to a chiropractor regularly, without a specific injury, then we likely still had a dental cavitation infection, root canal infection or dental implant infection.
X-Rays
Can an X-Ray show a hidden dental infection? X-Rays can show areas of bone and areas of non-bone. They are pretty useful for spotting dental cavitation infections, or holes in the bone where teeth have been extracted. Often the outline of the periodontal membrane (that was not properly extracted) can be seen. X-Rays do not show for sure if the area is infected, or if the infection causing symptoms. Similarly for X-rays looking for root canal infection, they can show where there is bone, but not necessarily if the area is infected or not.
Here is a panograph of my mouth before having dental cavitation surgery.
 ”
”
The areas of possible dental cavitation infection are where my wisdom teeth were extracted 25 years ago. I have no root canals. Looking closely at the X-ray, I can see the white lines that form circles where the wisdom teeth used to be, especially on the lowers. The bone clearly did not grow to fill in these pockets. But, are they actually infected? I have heard from a local oral surgeon that the Cavitat Ultrasound Scanner is much better than X-rays at accurately locating a dental cavitation. However, the question still remains. Are those holes actually infected? If so, will the resolution of the dental cavitation infections resolve any of my symptoms?
I saw three practitioners to get their opinions. One dentist said they’re probably infected because there’s clearly no bone growth in that area in the X-rays. Chances are there is some nasty bacteria, virus or yeast in there. Another dentist used muscle testing (similarly to what I’ve learned to do at home) and said they were infected (See Self Testing below for more details). The final practitioner, an MD in St. Louis, used Acupuncture Meridian Assessment (AMA) to determine if they were infected by looking for unbalanced acupuncture meridians. His opinion was that all four wisdom teeth extraction sites had dental cavitation infections.
My general opinion is that dental cavitation holes are most likely infected. If it is not already infected, there is a decent chance that some day a spirochete bacteria will bore into them and start an infection. If there are symptoms along the corresponding Meridian on the chart, and if a dental cavitation hole is present on an X-Ray, then I would consider treatment.
Now on to my husband’s possible root canal infection:

Could there be an infection in this root canal? No dentist or practitioner could point to anything in the X-Ray to indicate an infection. I don’t see anything either.
However, according to both the AMA and our Self Testing, the answer was yes. My husband had no symptoms that he was complaining about. He knew some of the literature and articles about root canals commonly being infected. He did notice that the root canal tooth seemed to migrate up and down depending on the weather and season of the year. This was a red flag in my book that there must be a root canal infection! After the MD’s AMA testing said it was infected, he finally gave in and had the tooth pulled. More on that later.
Thermal Imaging & AMA
Dr. Simon Yu, MD, uses thermal imaging of the face and Acupuncture Meridian Assessment (AMA) as indicators of dental infection. Thermal imaging isn’t a 100% diagnostic tool, he said, but it gives him some clues. He looks for asymmetries in the thermal image as indicators that there might be a hidden dental infection.
The AMA machine measures the DC impedance along the acupuncture meridian. Dr. Yu probed various acupuncture points while I held a ground probe in my other hand. He noticed disturbances in the dental meridians, which is a point found at the base of the thumb. He debugged which area by having me put the fingers of my grounded hand in my mouth at the areas where the wisdom teeth used to be. He found the most disturbance at #17 and #32, the two lowers. He put an antibiotic on the tray of his AMA machine to see if that balanced my meridian. Sure enough, the meridian balanced with the antibiotic and he concluded dental cavitation infections. He recommended conventional dental cavitation surgery (without ozone) for #17 and #32.
Later, my dentist convinced me that if some of the dental cavitations are infected, then they probably all are. He suggested dental cavitation surgery on all the wisdom teeth extraction sites. I later went back to the MD and he re-tested and found smaller disturbances on #1 and #16. I ended up having dental cavitation surgery on all 4 wisdom tooth sites. The decision was also made easier for me because of Lyme disease. I know that spirochete infections can bore into dental cavitations, hide there, and then re-appear later. After all my hard work on Lyme disease, I wanted to minimize any chance of it continuing to bother me.
Dr. Simon Yu uses AMA as previously described to diagnose hidden dental infections. I have learned to do AMA at home with a voltmeter, but I find that the acupuncture points are difficult to find. This method requires constant practice, and Dr. Yu is very good at it. I have also found AMA not as sensitive as Self Testing.
Self Testing
Through all of this dental experience, I have learned a variation on muscle testing to test for hidden infections at home. This has been consistent so far with the previous methods of testing and also with our clinical results. It is easier to do at home and takes less experience than AMA. I have also found it to be more sensitive than AMA. For example, we saw Dr. Yu after my husband’s root canal tooth was pulled and he said everything looked OK. Immediately after the visit, my husband got a phimosis infection. This prompted me to re-test Tooth #9, and I found signs of infection. Since the root canal tooth was gone, it was the beginnings of a dental cavitation infection. Based on this single experience, I’m suspicious that my home muscle testing is more sensitive in detecting hidden dental infections than AMA.
The other advantage of self testing is it offers some indication of if the bothersome symptoms are coming from the dental infection. What?!?! The AMA machine will tell you if there is an infection. It won’t really tell you, however, if the infection is causing your headaches, backaches, etc. A specific part of the body, like the head or the back, can be held in self testing. The other hand can go to the suspected tooth area. Weakness indicates the tooth is causing the head or back issue.
So how do I self test for hidden dental infections? The best way I can demonstrate the techniques is with example videos. Check out the ‘Overview of Debugging Methods’ video first if these debugging methods are new.
Summary – Diagnosing Hidden Dental Infections
Here is a summary of the strategy I use to figure out if there is a hidden dental infection:
- Check out the Tooth Organ Chart. See if any of the symptoms correlate with a particular tooth.
- Muscle test to see if I can find a possible infection in the tooth or problems in the area found in #1. (See above videos for examples)
- If there is a suspected dental cavitation infection in an extracted tooth socket, take an X-Ray to see if a hole surrounded by bone can be found. This is a sanity check. An X-Ray will usually be required by an oral surgeon or dentist before dental cavitation surgery anyway.
- Keep testing periodically – due to the adaptive nature of bacteria, infections can sometimes re-appear, or emerge when the body undergoes some kind of stressful event. If I have previously found an infection in a given tooth or area, I re-test pro-actively every 3-4 months.
Treatment for Dental Infections
Unfortunately bacteria in dental infections can adapt and mutate in extreme environments. They can change their shape and size, move from one place to another, and thrive in the absence of oxygen [1]. They can encyst and hide in the three miles of dentinal tubules in a tooth. They can live in the anaerobic environment of a dental cavitation hole surrounded by bone. Our immune system hopefully kills the infection as it tries to spread to the rest of our body. However, the immune system can’t access areas with little or no blood flow. Neither can antibiotics. This is why oral or IV antibiotic therapy generally won’t work on hidden dental infections.
We have tried for years and spent thousands of dollars on homeopathics, herbals, supplements, acupuncture, skin brushing and other therapies to treat dental infections. This was even before we realized that our symptoms were being caused by our mouths. Unfortunately all of these turned out to cover up symptoms. None of them got to the root of the problem. The following sections summarize our tips and lessons learned the hard way.
Root Canal Infection & Dental Implant Infection Treatment
I get this question often: What do I do if I have a root canal infection or dental implant infection? Then come the follow on questions: Can the infection be treated with ozone alone? Do I really have to extract the tooth? Should I do a bridge or a partial after extraction? Let’s start with a summary of lessons learned from the trenches of dental disaster:
- First, I would try a few ozone injections. Ozone injections might give a sense if the symptoms are coming from the hidden infection or not. The practitioner should be able to drill and place a tap around the infected tooth. The ozone gas syringe can be connected to the tap. Typically 2-12cc’s are injected, depending on the location and tolerance of the patient. After the ozone injection, if the symptoms change in either direction (worse or better) then the hidden infection is the likely culprit. If the symptoms don’t change, then it could be something else as the primary cause of the symptoms. Any changes should be pretty immediate, within 24 hours. Sometimes ozone injections can relieve symptoms for a longer period of time. It is possible that periodic ozone injections might be enough to relieve symptoms enough to live well. For these people, ozone injections a few times per year might be enough. It’s possible. Note that I don’t think ozone injections alone will get rid of the infection completely. There are 3 miles of hiding places for bacteria in a root canal tooth, and plenty of hiding places in a dental implant as well.
- If ozone injections don’t help for a longer period of time, then I would prepare for tooth extraction:
- First, I would get a few osteopathic treatments to make sure the cranial bones are in the best alignment possible.
- Eat well, sleep well, de-stress. Check for vitamin and mineral deficiencies (we use ZYTO to check). Get the immune system and overall health into the best shape possible. Once the infection is disturbed and released into the body, the immune system needs to be strong. My personal opinion is to take orally at least 4g Vitamin C and 10kIUs Vitamin D3 starting a week before extraction.
- Find an oral surgeon or dentist who does extractions using ozone. This is extremely important. I would not risk the surgery with someone who doesn’t use ozone. Equally important is to make sure the practitioner is educated about removing the periodontal membrane. If they don’t remove it, bone won’t grow, and a dental cavitation infection is more likely to form.
- Use ozone before, during and after the extraction to help prevent infection. Rinse & spit with ozone water for several days after any dental surgical procedure. We bubble the water at home or in the surgeon’s office with this ozonator. My second choice to ozone would be hydrogen peroxide.
- Extract the tooth.
- If available, get a Vitamin C IV right after extraction. If not, increase Vitamin C and D to help the immune system.
- Drainage, detox and healing support. The body must heal the surgery site and dealing properly with any viruses or bacteria that have either died or been displaced. Test possibilities via ZYTO if available. If these are not available, then test by holding the remedies up to the tooth area. We tested hundreds of remedies after dental surgery at home and through ZYTO. The top four testing well for me after surgery were: Body Mend, Dental Chord, Kidney Tone and Bacteria Chord. About 3-4 weeks later I shifted to testing best on Body Mend, Lymph Tone III and Adrenal Terrain. Body Mend consistently tested well, up to 7 months post surgery. Below is an example video of the testing methodology I used to figure this out.
- Follow extraction by a series of at least 6 ozone injections in the surgery site over the next few months. This is to prevent future dental cavitation infections in the area.
- So what do I recommend after the tooth is extracted? A bridge or a partial. Even once the bridge or partial is in, don’t forget those ozone injections to prevent a dental cavitation infection. The practitioner can drill an ozone tap into the bone above the bridge. The bridge has the disadvantage of filing down the neighboring teeth. Structurally, those teeth need to be able to support the bridge for a long time. A partial has to be taken out and cleaned, and is not always as secure while eating in the mouth. There is no perfect solution, unfortunately. If the tooth crosses the Cranial Midline (#8, 9, 24, or 25), then see below for more information about midline bridges.
Sorry for the bad news. Really, really sorry. Unfortunately we don’t currently have the ability to sterilize the 3 miles of tubules in teeth. The likelihood of the root canal infection still being there is pretty high.
There are also currently no practitioners who can do dental implants without infection. I have tested a few people with dental implants and I have always found them to be infected. There are several practitioners making the same observation. The people I have tested who got ozone injections did feel better. Dr. Klinghardt is supposedly working with a few dentists on a new implant technique that won’t harbor infection. I have yet to hear independent confirmation that they have been successful. In my experience, implants are about as likely as root canals to be infected. So for now, I would extract the tooth and do a series of ozone injections following the extraction, as outlined above.
I have heard the argument from some Osteopaths that dental implants should be used because otherwise they imbalance the jawbone and overall cranial structure. My recommendation is to get osteopathic treatments before tooth extraction to make sure the cranial bones are in the best alignment possible. I would also get treatments before and after a bridge or partial is placed.
Now, on to finish the story of my husband’s tooth #9, a root canal infection. Remember, he had no pain at all in the tooth, and was only considering doing something because several dentists, his wife, and an MD told him it was infected (details above). My husband finally had his front tooth extracted and replaced with a bridge (see notes below about dangers of a midline bridge! Oh, how I wish we had been more educated about this topic…). His back immediately felt better, his brain fog cleared up, he had more energy, and most importantly, he did twice as much housework. Immediately after his extraction, I tested for infection and it appeared to be gone.
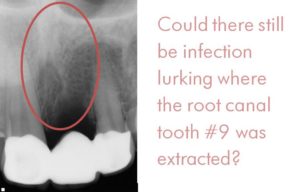
About 4 months later, after a phimosis infection, I re-tested for infection. The area above tooth #9 was testing as being infected again. After all his pain and suffering to extract the tooth, I didn’t want a dental cavitation infection to form. I sent him to the dentist, and her energy testing with a slightly different method came out positive as well. He swore again that he had no symptoms and the tooth socket could not possibly be infected. I sent him for an ozone injection, kicking and screaming.
After the first ozone injection, he said the bridge area felt more stable and he was more comfortable biting and chewing. He again said that his back felt better. He didn’t notice much difference after the 2nd ozone injection, and he was testing infection free thereafter. However, I haven’t given up the possibility that the infection is still hiding and that it won’t resurface. I still test him every few months.
Dental Cavitation & Extracted Teeth
What is my opinion about treating dental cavitations? Traditional dental cavitation surgery with an oral surgeon who uses ozone. Follow this by at least 6 ozone injections into the surgery site over the next few months. Similar to my comments about ozone injections for treating root canal infections, I don’t think ozone injections alone are going to solve dental cavitation infections permanently. Trying an ozone injection first is a decent idea, for two reasons:
- Ozone injections might give an idea of if the symptoms are coming from the hidden infection or not. The practitioner should be able to drill and place a tap into the dental cavitation. The ozone gas syringe can be connected to the tap. Typically 2-12cc’s are injected, depending on the location and tolerance of the patient. After the ozone injection, if the symptoms change in either direction (worse or better) then the hidden infection is the likely culprit. If the symptoms don’t change, then it could be something else causing the symptoms. Any changes should be pretty immediate, within 24 hours.
- Sometimes ozone injections can relieve symptoms for a longer period of time. It is possible that periodic ozone injections might be enough to relieve symptoms enough to live well. For these people, ozone injections a few times per year might be enough. It’s possible. If you’re one of these lucky people, Live On! Note that I think the likelihood of ozone injections alone totally getting rid of the dental cavitation infection is low.
So why traditional dental cavitation surgery? The area needs to be cleaned out completely. Removal of the periodontal membrane during traditional cavitation surgery means that bone can now form where the hole once was. This surgery will bring blood flow to the area, which means the immune system will arrive to the scene. The immune system is our best defense against any bacteria, virus and yeast that the practitioner didn’t clean out. Ozone injections alone won’t achieve bone growth in the hole. But they might (temporarily) relieve symptoms of the infection.
Before dental cavitation surgery, I tried all kinds of things. Mouthwashes, herbals, homeopathics, acupuncture, oil pulling. I found them all to be ‘symptom cover-ups.’ I sometimes got relief or felt a little better, but none of the results were lasting. Dental cavitation surgery was necessary for me to finally experience permanent symptom relief. I had no idea how good I could feel until after the cavitations were finally resolved!
What if you are waiting for dental cavitation surgery? Is there anything that can help reduce symptoms, even temporarily? Ozone injections are worth a try. I did also find clinically that sesame oil pulling seemed to help me feel better. I’m guessing oil pulling helped me detoxify and drain the infections as they tried to spread beyond the cavitation hole. After resolution of my cavitations, oil pulling didn’t make me feel better anymore. I can’t say whether or not this is a general result- I don’t have enough data points. It’s also possible that swishing the mouth with other anti-microbials or binders might work equally well. Note that I did not get any real symptom resolution from oil pulling, I just felt slightly better overall.
Now, on to my story and lessons learned from dental cavitation surgery. I had traditional cavitation surgery on all four of my wisdom tooth sites. The operation was performed by an oral surgeon (my understanding is that this is typically a covered procedure under medical insurance). The details of the mishaps can be found here. Suffice it to say that the oral surgeon did not use ozone, and this was a very big mistake! Furthermore, he drilled from the cavitation site up into the sinus area, puncturing the sinus membrane. Another big mistake. I ended up with a septic infection on the whole left side of my face. A local dentist ended up saving my life with ozone injections. It turned out that all four of my cavitation sites were still infected after surgery! I needed about 6-8 ozone injections in all of the surgery sites.
About a year later, I was having constant chiropractic issues on my left side. It felt like I was locked up from the occiput all the way down to my tailbone. This feeling was on my left side only, my right side felt great. I also had variable ringing in my left ear, but my right ear was totally quiet. I went to about 10 chiropractors, all of whom had different treatment styles. They all relieved my locked-up feeling, but only for about 1-2 days. It kept coming back. Another trip to visit Dr. Simon Yu, MD, and he found that wisdom tooth socket #17 was still infected. It turns out that Tooth #17 had a larger cavitation than it did before I had the first cavitation surgery! It needed to be re-opened and cleaned out again. This time I did my research and had oral surgery where the office uses ozone to prevent infection. This surgeon also did PRF (platelet-rich fibrin) to help the socket heal. I had an interesting experience during this dental cavitation surgery. I could hear and feel him scraping, ozoning, suctioning deeper and deeper into the hole. At one point, I felt my left side release from the occiput all the way down to the tailbone! My left-side-lockup problem released right in the surgery chair! After this surgery, I again had a series of about 8 ozone injections in the area.
After five total dental cavitation surgeries, I have some lessons learned and tips to share. I have written a Cavitation Surgery article which has a printable Cavitation Surgery Checklist. Definitely check those out if you decide to do the surgery. If you’re still trying to decide and want to get a feeling, here are a few of the important points from the article:
- Traditional dental cavitation surgery might be able to be prevented all together with ozone injections. Try those first! In hindsight, I had 2 dentists, 1 MD and 1 oral surgeon all tell me that I probably didn’t need cavitation surgery on the upper wisdom teeth sites (#1 & #16). I might have gotten enough symptom relief with periodic ozone injections alone in those areas.
- Find a practitioner who will use ozone during the surgery. Dental cavitation surgery is too risky to use a practitioner who doesn’t use ozone. My second oral surgeon described his technique to me as follows: Drill, scrape, ozone, drill, scrape ozone, keep repeating until the ozone stops bubbling.
- Find a practitioner who does PRF (platelet-rich fibrin) after the cavitation surgery. I seemed to have better results with PRF than without.
- Ask in advance if they will force your mouth open during surgery. The dental assistant did this to me during my first cavitation surgery. Trismus is very painful and difficult to resolve.
- Don’t let anyone drill into the sinuses through your mouth. The first oral surgeon did this to me, and I ended up with major chiropractic and osteopathic issues for many months because there was still infection in the sinus area. This was in addition to becoming septic on this side of my head with a sinus infection, ear infection, jawbone infection, and eye infection. Just in case this does happen to you, here are some quick tips for a deep sinus membrane infection: Nasal ozone 30 min 2x/day bubbled through olive oil. Ear ozone 30 min 2x/day bubbled through olive oil. Ozone injections into the sinus acupuncture points in the neck – on the order of 1cc at about 25 gamma. (Note: need medical grade ozone setup is needed for the latter).
- Preparation for Dental Cavitation Surgery – First, I would get a few osteopathic treatments to make sure the cranial bones are in the best alignment possible. This will help ensure that the body can detoxify, drain and heal. Then, I would be sure to Eat well, sleep well, de-stress. Actually, one should do these all the time, but especially while preparing and recovering from cavitation surgery. Check for vitamin and mineral deficiencies (We do this with ZYTO. Get the immune system and overall health into the best shape possible. Once the infection is disturbed and released into the body, the immune system needs to be strong. My personal opinion is at least 4g Vitamin C and 10kIUs Vitamin D3 starting a week before extraction.
- Use ozone before, during and after the procedure to help prevent infection. Rinse & spit with ozone water for several days after any dental surgical procedure. We bubble the water at home or in the surgeon’s office with this ozonator. My second choice to ozone would be hydrogen peroxide.
- After cavitation surgery, get ozone injections into each surgery site, starting about 7 days after surgery. Reference [1] is another case where even after cavitation surgery, there are still multiple infections – this time even deeper and more difficult to treat. How many ozone injections are needed after surgery to prevent recurrence? We don’t know, but my bets are on 6-10 injections spaced over 6 months after surgery. We know that microscopically it takes over 1 year for bone to fill in a cavitation.
- Drainage, detoxification and general support after cavitation surgery – This was to make sure my body was healing the surgery site and dealing properly with any viruses or bacteria that had either died or been displaced. I would test possibilities via ZYTO if available. If not available, then I would test by holding the remedies up to the tooth area. Dental Cavitation Infections, Cranial Midline, and Frenulum Check is an example video of the testing methodology. I tested hundreds of remedies after cavitation surgery in my garage and ZYTO database. I even made a homeopathic remedy out of a sample of the infection. The top four testing well and clinically helping me after surgery were: Body Mend, Dental Chord, Bacteria Chord. About 3-4 weeks later I shifted to testing best on Body Mend, Lymph Tone III and Adrenal Terrain. Body Mend consistently tested well, up to 7 months post surgery. If I could do it again, I would also try swishing Asea water. Several friends have had good results with it in healing from dental surgery. I also tested and tried some of Louisa Williams suggestions. I did not find any of them testing well or helpful. Additionally, her suggestion of the laser sounds dangerous if the detoxification and drainage pathways in the body are stuck.
- Vitamin C and Vitamin D – These offer general support for the immune system after dental procedures. In addition to Liposomal Vitamin C, I did get several 30g Vitamin C IV drips after cavitation surgery (and I still went septic after the first one!). I do recommend the IV if possible, if not then the oral Vitamin C.
- Dental DNA – Some practitioners offer to send samples to Dental DNA for identification. I didn’t do this. Why? I knew already there are all kinds of nasty bacteria, viruses, and yeast in there. Giving them a name doesn’t help me. If I really wanted to name them, I would go to ZYTO after surgery. ZYTO has the advantage of also finding other issues, and giving a treatment that might help the body drain, detox, or methylate. Dental DNA is not covered by any insurance, to my knowledge, at this point in time. I did, however, get a sample of the infection and made a homeopathic remedy from the sample. Unfortunately, this didn’t test well, and the support items listed above were much more valuable.
Dental cavitation surgery is no fun. There’s no hiding that fact. However, after five dental cavitation surgeries, I can say it was worth it. Permanent Symptom Resolution + More Vitality Overall = Priceless.
Midline Missing Tooth Options
My husband made the HUGE mistake of putting in a bridge after tooth #9 was extracted. The problem with such a bridge is that it crosses the cranial midline. This basically fuses two cranial bones together that were meant to have a few millimeters of wiggle room. Restriction of cranial motion across the midline can create worse symptoms than the original dental infection itself [4]! If an extraction is needed on a midline tooth #8, #9, #24 or #25, then here is my assessment of the options:
- Cantilever bridge – it seems like each dentist has a unique take on how to do a cantilever. Basically this is a bridge with flexibility around the midline. It is unclear, however, how structurally stable this bridge is over the long term. The two teeth next to the missing tooth need to be filed down, potentially compromising their stability.
- Implant – I have seen some dentists educated in cranial issues recommend implants. Unfortunately I believe that most dental implants also harbor hidden infections. I have tested a very small number of people with implants and I have always found them to be infected. The people I have tested who got ozone injections did feel better. This is only my experience on a small sample size, but this coupled with several practitioners’ similar opinions make me very wary of implants. Klinghardt is supposedly working closely with a few dentists to develop a better implant technique that avoids infection. If for some reason I really wanted an implant, I would travel to work with Klinghardt’s dentists. I would definitely follow the procedure with a series of 6 or more ozone injections around the site.
- Partial – This option has the advantage of being able to take it out at night. It may not be as secure in the mouth, especially when eating. I would work with an osteopath to make sure that the partial is not effecting cranial structure or function while it is being worn.
- ALF with tooth – This is an interesting option proposed to me by an osteopath. The ALF is expensive, but it is specifically designed to support alignment of the bones using principles of cranial osteopathy. Apparently they can attach a tooth to the ALF appliance, basically turning it into a partial. The difference is that this ‘partial’ is specifically designed to support proper cranial function. An expensive solution, but worth considering.
So what would we do if we could do my husband’s Tooth #9 all over again? A partial. This doesn’t fuse the cranial bones together. This option also doesn’t require the neighboring teeth to be filed down.
Case Study of a Friend – Swollen Eyes = Dental Infection?!?
My good friend had cracked tooth #11, broken her foot, had painful knees, brain fog, and swollen, painful eyes. She went to a dentist who fixed her tooth with a screw & bridge. She went to urgent care and a podiatrist and got a boot for her foot. She went to an orthopedic doctor to get cortisone injections in her knees. She went to the opthalmologist and got drops and antibiotics for her swollen, painful eyes.
I suggested that tooth #11 might be a hidden root canal infection. She thought I was crazy. Finally one day she desperately called me and said her eyes were so painful, nothing was helping, and she was willing to try anything. I tested and sure enough, tooth #11 was infected. I sent her to a dentist, who confirmed my suspicion with her own energy testing methods. My friend got an ozone injection, done by drilling a tap into the bone above tooth #11 and then injecting ozone gas. The immediate resolution of her swollen, itchy eyes was astounding! Here are pictures of her immediately before and immediately after her ozone injection in the waiting room of the dentist’s office:

This friend has gone on to get about 10 more ozone injections so far. I am skeptical that these will permanently resolve the infection, since she has several root canals and a few posts in the area. This means that there are lots of places for the infection to hide, and then reappear later. Taking out these teeth would essentially mean dentures for her, so understandably she doesn’t want to take them out. It’s possible that she’ll just need ozone injections a few times a year, or maybe even once every few years or so. I’ll report back as this case evolves.
FAQ
Q: How many ozone injections do you need to clear up a dental cavitation infection, root canal infection, or dental implant infection?
A: It seems to depend on the situation. If the tooth or periodontal membrane are still in place, then the chances of completely eradicating the infection are low. The infection can hide and re-appear later. My guess as to the timeline of possible reappearance is anywhere from months-years. If we are talking about a properly extracted tooth, I have heard estimates from 4-8 injections. In our experience, it took 5 injections for my husband’s tooth #9 after extraction and about 8 injections on my wisdom teeth sockets AFTER I had already had cavitation surgery.
Q: Will insurance cover the cost of ozone injection treatment?
A: It depends on your insurance. In our PPO insurance case, they did not cover ozone injections from our dentist. However, they did partially cover it from an oral surgeon.
Q: Will insurance cover the cost of tooth extraction or dental cavitation surgery?
A: It depends on your insurance. In our PPO insurance case, they did cover all of the surgeries. One practitioner said he needed to send a biopsy for them to cover the cavitation surgery. Later, another practitioner did not do a biopsy and it was covered anyway. This probably also depends on the insurance.
Q: Are there any daily dental hygiene suggestions for preventing future infection after surgery?
A: Immediately after surgery, I would rinse and spit with ozone water. My second choice to ozone would be hydrogen peroxide. I would continue rinsing and spitting daily for at least 2 weeks after surgery. After bone grows near the surgery site, it seems unlikely that viruses and bacteria can bore through bone from the mouth and create another infection. Blood flow after surgery from the other side should be good, assuming the periodontal membrane was removed. We do know that microscopically it takes at least a year for a dental cavitation or extracted tooth socket to fill in with bone. So my conclusion/opinion? Until I can feel bone at the surgery site, I would continue the ozonated water or hydrogen peroxide swishing.
Q: Are there any daily dental hygiene suggestions for preventing infection in general?
A: The best suggestion I have is to change the diet. We’ve found it quite difficult to get cavities if you don’t eat sugar. Our daily dental hygiene is floss & brush with aluminum-free baking soda twice per day.
References
[1] Dr. Simon Yu MD, “Wisdom Teeth Undetected Tooth Infections and Incurable Medical Symptoms”
[2] George Meinig DDS FACD, “Root Canal Cover-Up”
[3] http://diagnosisunsolved.com/2014/07/healthy-on-the-inside/
[4] Dr. Gerald H. Smith, “Dental Bridgework May Be the Source of Your Patients’ Headaches, Neckaches and Facial Pain.”
[5] http://www.hugginsappliedhealing.com/
[6] Hal Huggins DDS MS, “Root Canal Dangers” 2010.
[7] B. Windham“Incidence Levels and Chronic Health Effects Related to Cavitations”
[8] Weston A. Price MS DDS FAGD, “Nutrition and Physical Degeneration,” 1939.
[9] Robert Kulacz DDS & Thomas Levy MD, The Toxic Tooth: How a root canal could be making you sick , Nov. 2014.
Was this information useful? If so, please consider donating to keep this site alive.
Last Updated: